Cost of Delivering a Baby Cost of Annestesia
- Review
- Open up Admission
- Published:
Anesthesia for cesarean commitment: general or regional anesthesia—a systematic review
Ain-Shams Journal of Anesthesiology volume thirteen, Article number:ane (2021) Cite this article
Abstruse
Groundwork
Full general anesthesia and regional anesthesia are the anesthetic techniques of choice for cesarean delivery. These anesthetic techniques take their furnishings on both the fetus and mother. The selection of anesthetic techniques for cesarean delivery depends on several factors including physiological presentation of the patient, feel level of the practitioner, availability of drugs, and equipment, amidst others. Nevertheless, whichever technique is used is chosen because of its safety contour and benefit to both mother and fetus. Therefore, this study aimed to compare the furnishings of general anesthesia against regional anesthesia on fetal and maternal outcomes for cesarean commitment.
Main body
Search methods were conducted on PubMed, Scopus, Embase, and Cochrane library to identify eligible studies using the keywords, MeSH terms, and filters. 2 review authors independently assessed the included studies for quality, bias, and accurateness. A total of fourteen (14) studies (1924 women) contributed information for this review. Findings showed that the 1st and 5th infinitesimal Apgar scores were higher in regional anesthesia than in general anesthesia while the 1st minute Apgar scores < 7 were more in general anesthesia. On the other hand, fetal umbilical arterial blood pH was lower in regional anesthesia. Also, intraoperative hypotension was more in regional anesthesia while middle rate and estimated blood loss significantly college in general anesthesia.
Conclusion
In conclusion, regional anesthesia emerges every bit a better option evidenced past its meliorate fetal and maternal outcomes. All the same, both regional anesthesia and full general anesthesia are still used for cesarean delivery.
Background
Cesarean delivery can be performed as either constituent or as an emergency. Globally, there is an increasing proportion of women giving birth by cesarean delivery in both adult and developing countries which is either washed by the adult female's asking or as a result of complications (Ghaffari et al. 2018). The rate of cesarean delivery in the United states is reported to be around 30% of all live births and 25–30% in Columbia (Páez and Navarro 2012). Also, it has been reported by Footling et al. (Lilliputian et al. 2016) that the U.s. has a college rate of cesarean commitment around 65%. An essential footstep in the choice of coldhearted technique for cesarean delivery is the safety and wellness benefits to the mother and fetus. With the advancement of anesthesia techniques, operations have become safer and secured over the years, but significant maternal and fetal mortality and morbidity (Sumikura et al. 2016) do exist. Anesthesia for cesarean commitment can exist accomplished either through general anesthesia (GA) or regional anesthesia (RA) such as spinal anesthesia (SA), epidural anesthesia (EA), or combined spinal-epidural anesthesia (CSE).
Regional anesthesia especially spinal anesthesia has been favored equally the all-time choice for elective unproblematic cesarean delivery due to its avoidance of the airway, less take chances of aspiration of gastric content, and easy to perform (Shibli and Russell 2000; Kim et al. 2019). Regional anesthesia is prophylactic and effective, but it does have complications such every bit hypotension, local coldhearted toxicity, post-dural puncture headache (PDPH), and nerve damage (Bakri et al. 2015; Bloom et al. 2005; Afolabi and Lesi 2012; Aregawi et al. 2018). However, general anesthesia is still used specially when regional anesthesia is contraindicated or failed. Advantages of full general anesthesia include maintained patent airway, controlled ventilation, and less cardiovascular low (Devroe et al. 2015). Complications such as failed intubation, failed ventilation, aspiration of gastric content, awareness, pain, and fetal depression (Yehuda Ginosar et al. 2013) are common in GA.
The essence of anesthesia for cesarean delivery is the safe delivery of the fetus and less or no complication to the mother. Therefore, it is important to compare both fetal and maternal outcomes associated with regional anesthesia and general anesthesia.
Several studies have made the attempt to compare fetal outcomes (1st and 5th minute Apgar scores, arterial blood pH) (Kolås et al. 2007; Sabol and Caughey 2016) and maternal outcomes (blood loss, claret pressure and heart rate, analgesia use and requirements) (Kimber Craig 2019). Two studies reported no divergence in the 5th minute Apgar score between regional anesthesia and general anesthesia but concluded by stating that no sufficient evidence exists to prove that regional anesthesia stands superior to full general anesthesia (Kim et al. 2019; Afolabi and Lesi 2012). Nevertheless, other studies accept reported that regional anesthesia is superior to general anesthesia in terms of fetal Apgar score and umbilical arterial blood pH (Kim et al. 2019; Nguyen-Lu et al. 2016).
Aim of the study
The aim of this systematic review was to compare the furnishings of general anesthesia with regional anesthesia on fetal and maternal outcomes for cesarean commitment. The fetal outcome variables were 1st and 5th minute Apgar scores and umbilical arterial claret pH while the maternal outcome variables were blood loss, blood pressure and heart charge per unit, and analgesia requirement.
Principal text
Fabric and method
A systematic review study was conducted. A search strategy was used to search on PubMed, Embase, Scopus, and Cochrane using keywords, MeSH terms, and filters equally shown in Tabular array 1. Randomized clinical trials and observational studies that compared the furnishings of general anesthesia and regional anesthesia on maternal and fetal outcomes during cesarean delivery were included. The included studies were reported according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA). All the included studies were subjectively and independently assessed for adventure of biases (Fig. 1) by ii authors (MI, ZHK) using the bias domain described in the Cochrane Handbook for Systematic Review of Interventions version v.three.5 (Higgins et al. 2019). All included studies were assigned a judgment of "high," "low," or "unclear" risk of bias across the post-obit domains: random sequence generation, allocation darkening, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting. Disagreements were resolved by a discussion between the two assessors and a third outside assessor (SWJ), who provided arbitration. Data extraction was independently done past the authors, and discrepancies were resolved through a consensus give-and-take.
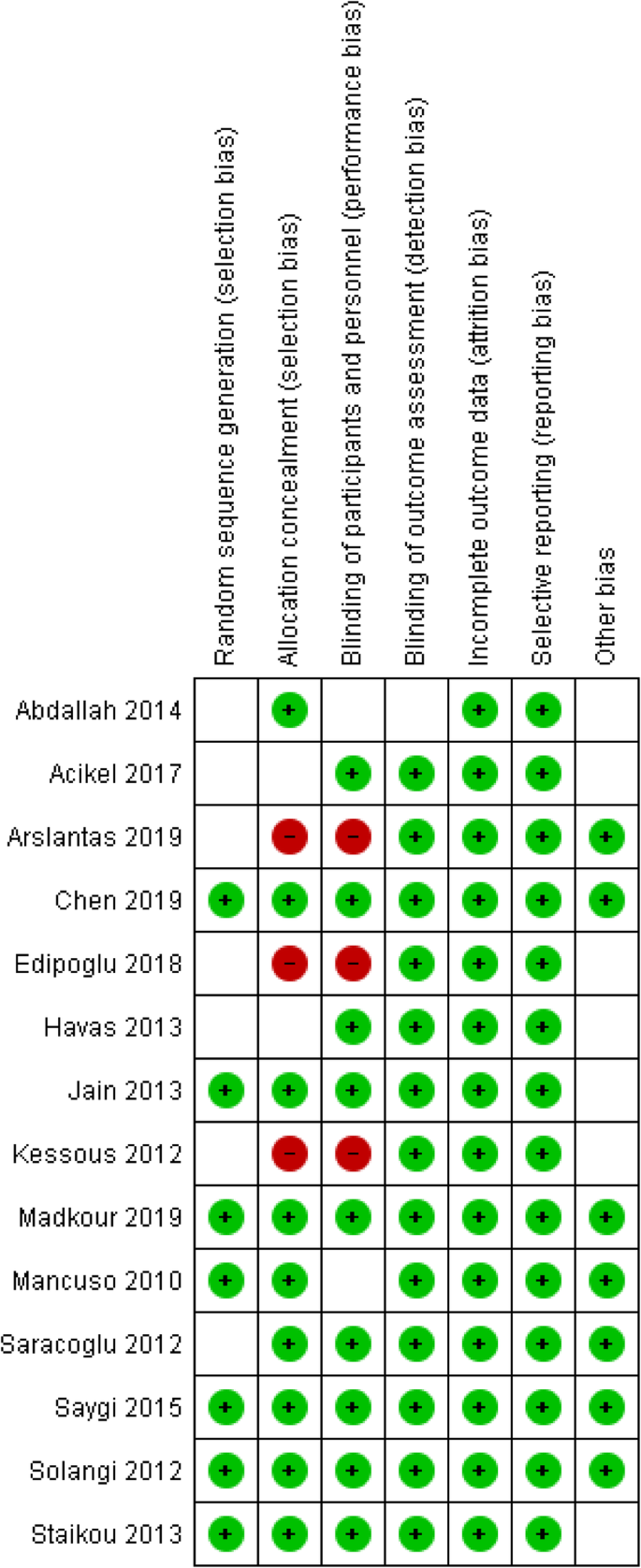
Assessment of take chances of bias of all included studies
Study selection
The search results and reasons for exclusion from the study are shown in Fig. 2. Initially, we screened a total of 2538 articles from PubMed, Embase, Scopus, and Cochrane. We had 476 duplicated studies removed, and 2003 articles non meeting the inclusion criteria were also excluded. The remaining 59 studies' total text was reviewed, and 45 studies were excluded due to the method and report design used. Finally, 14 randomized controlled trials and observational studies comparing general anesthesia and regional anesthesia were included.
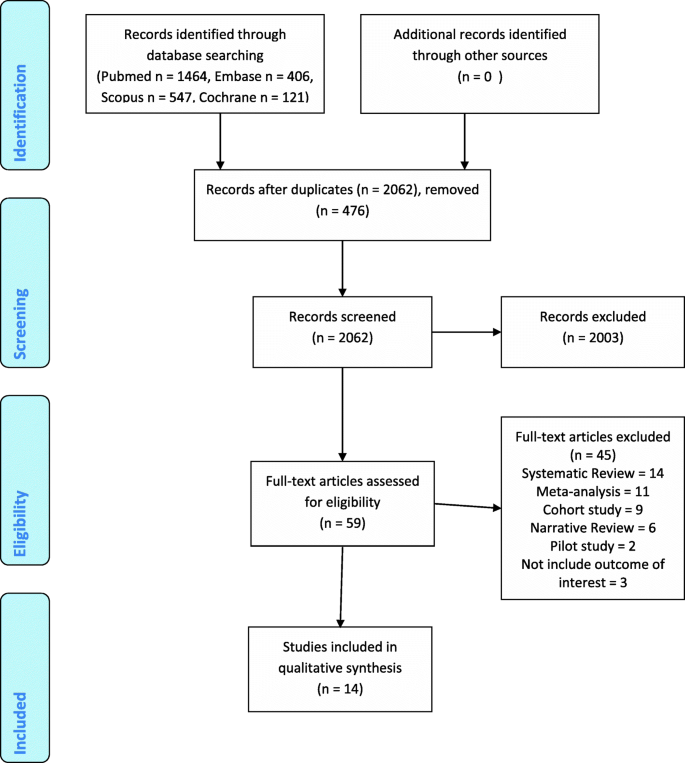
Prisma flowchart
Study characteristics
Characteristics of the included studies are detailed in Table 2. Fourteen studies (1924 parturient women) met the inclusion criteria. Nine of the included studies were randomized clinical trials (Jain et al. 2013; Chen et al. 2019; Saygi et al. 2015; Solangi et al. 2012; Mancuso et al. 2010; Staikou et al. 2013; Açıkel et al. 2017; Madkour et al. 2019; Saracoglu et al. 2012) and five prospective cross-sectional observational studies (Kessous et al. 2012; Edipoglu et al. 2018; Arslantas and Umuroglu 2019; Abdallah et al. 2014; Havas et al. 2013). Furthermore, ten of the included studies were conducted with parturient women scheduled for elective cesarean delivery (Jain et al. 2013; Saygi et al. 2015; Solangi et al. 2012; Mancuso et al. 2010; Staikou et al. 2013; Madkour et al. 2019; Saracoglu et al. 2012; Kessous et al. 2012; Abdallah et al. 2014; Havas et al. 2013), 2 studies on emergency cesarean delivery (Açıkel et al. 2017; Edipoglu et al. 2018), and the remaining two on both elective and emergency cesarean delivery (Chen et al. 2019; Arslantas and Umuroglu 2019).
Results
The 1st minute fetal Apgar scores between combined spinal-epidural and general anesthesia showed no meaning departure (8.98 ± 0.89, 9.01 ± 0.98, P value 0.863) (Chen et al. 2019; Abdallah et al. 2014). Nevertheless, the 1st infinitesimal Apgar scores of fetuses born to mothers exposed to spinal anesthesia were higher than those exposed to full general anesthesia (7.5 ± 1.seven, half-dozen.iii ± 1.12, P < 0.005) (Saygi et al. 2015; Solangi et al. 2012; Açıkel et al. 2017; Madkour et al. 2019; Edipoglu et al. 2018; Abdallah et al. 2014; Havas et al. 2013). This showed that babies who were recorded to accept lower fetal Apgar scores were likely to exist resuscitated or kept under close monitoring. Again, the number of babies with 1st minute Apgar scores < 7 was college in general anesthesia, followed by spinal anesthesia which was converted to general anesthesia and spinal anesthesia equally the to the lowest degree. Likewise, the median fifth minute Apgar scores > 7 were higher in spinal anesthesia followed by spinal anesthesia converted to general anesthesia and least in general anesthesia (Madkour et al. 2019).
No difference was plant in the fifth minute Apgar scores comparing between regional anesthesia and full general anesthesia, but the former had a better score (Chen et al. 2019; Abdallah et al. 2014; Havas et al. 2013). Besides, at that place was no difference between low-dose spinal and general anesthesia with regard to the 1st and 5th infinitesimal Apgar scores (Jain et al. 2013).
Regarding fetal umbilical arterial blood pH, only one of our included studies found a significant difference between regional anesthesia and general anesthesia. Umbilical arterial blood pH was lower (acidic) in regional anesthesia than in general anesthesia (pH seven.23 ± 0.06 and 7.27 ± 0.04, respectively) (Jain et al. 2013).
As function of the standard anesthesia protocols, blood force per unit area and heart rate are e'er monitored during surgeries. At that place were no significant changes in the blood force per unit area and heart charge per unit during the preoperative period (Jain et al. 2013; Chen et al. 2019; Edipoglu et al. 2018; Abdallah et al. 2014). However, intraoperative hypotension was more than in regional anesthesia (Jain et al. 2013; Chen et al. 2019; Saygi et al. 2015; Arslantas and Umuroglu 2019; Abdallah et al. 2014; Havas et al. 2013). Also, higher center rates were recorded in general anesthesia than in regional anesthesia (Jain et al. 2013; Chen et al. 2019; Madkour et al. 2019; Edipoglu et al. 2018). With hypotension recorded in regional anesthesia, more intravenous fluids were used than in general anesthesia (Havas et al. 2013) to prevent or reduce the hypotension. Again, the use of vasopressors like ephedrine (Staikou et al. 2013; Havas et al. 2013) and phenylephrine (Jain et al. 2013) to treat hypotension was higher (range 0–50 mg against 0–x mg) in regional anesthesia than in full general anesthesia.
Furthermore, at that place was a higher intraoperative analgesia requirement (2 μg/kg versus 20 μg of fentanyl) in general anesthesia (Kessous et al. 2012) while the first postoperative analgesia requirement fourth dimension was recorded to be longer in regional anesthesia (Saygi et al. 2015; Madkour et al. 2019; Saracoglu et al. 2012; Arslantas and Umuroglu 2019). For instance, the first postoperative analgesia requirement time in regional anesthesia was recorded to be 320 min, against 175 min in general anesthesia. This supports the loftier quantity of total fentanyl use in general anesthesia than in regional anesthesia (638 mcg fentanyl against 320 mcg fentanyl, respectively) (Saracoglu et al. 2012). Also, blood loss recorded was more (about 400 ml) in full general anesthesia (Chen et al. 2019) just did non accept whatsoever significant effect on the rate of claret transfusion. Render of bowel sounds and gas discharge took a longer time (9.vii ± 1.3, vi.viii ± 1.6 h, P = 0.001) in general anesthesia (Saygi et al. 2015; Madkour et al. 2019) while the showtime postoperative urine output was more than in regional anesthesia (Madkour et al. 2019).
As well, patients were more satisfied with regional anesthesia (Açıkel et al. 2017; Saracoglu et al. 2012) during cesarean delivery and would choose it again if the need arises. Reverse to this, one of our included studies showed that postoperative patient satisfaction was higher in general anesthesia (Chen et al. 2019).
Give-and-take
Similar to our findings, Dyer et al. (Dyer et al. 2003) in their study showed higher 1st minute Apgar scores in spinal anesthesia than in full general anesthesia with the 1st minute Apgar scores < 7 recorded more in general anesthesia. Also, no significant difference in the 1st and fifth minute Apgar scores was institute, but college 1st and 5th minute Apgar scores were recorded in regional anesthesia (Harazim et al. 2019; Shek et al. 2012). Information technology is clearly understood equally to why fetal asphyxia, fetal distress, depression, and resuscitation were recorded less in regional anesthesia as the babies were born very active. Caglar et al. (Caglar et al. 2013) in their study did not detect much deviation in umbilical arterial blood pH, but our findings showed a lower umbilical avenue claret pH (acidic) in regional anesthesia than in general anesthesia. This did not have any significant event on the infant because no cyanosis, body color modify, or respiratory distress, although no further investigations were carried out to find the course of low umbilical arterial blood pH.
As part of the maternal event, our findings did not show whatsoever pregnant deviation in blood loss betwixt regional anesthesia and general anesthesia. Therefore, patients who take regional anesthesia for cesarean delivery are less probable to receive a blood transfusion, unless there is an underlying condition or complications which may either occur before or after the procedure. Aksoy et al. in their study demonstrated that regional anesthesia was associated with less chance of operative claret loss and transfusion. Even so, in low-hazard patients, four patients (2%) nether full general anesthesia received nine units of blood transfusion (Aksoy et al. 2015).
Khan et al. (Khan et al. 2019) stated that hypotension was common in spinal and epidural anesthesia. Similar to our findings, astringent intraoperative hypotension was college in regional anesthesia. Aregawi et al. (Aregawi et al. 2018) stated that the vasodilation and venous pooling effects of the local anesthetic drugs used for regional anesthesia resulted in severe hypotension. Hypotension was treated with intravenous fluids, phenylephrine (Nguyen-Lu et al. 2016), and ephedrine (Bakri et al. 2015; Dyer et al. 2003). However, Kim et al. (Kim et al. 2019) stated that fetal umbilical arterial blood pH was adversely affected by the utilize of ephedrine. This explains why babies whose mothers had received greater ephedrine were found to accept low umbilical arterial blood pH (acidic).
Furthermore, the first postoperative analgesia requirement time was longer in regional anesthesia while the postoperative total analgesia consumption was higher in general anesthesia which is in coinciding with the other studies (Páez and Navarro 2012; Bakri et al. 2015; Afolabi and Lesi 2012). Patients were more satisfied with regional anesthesia as they could see the surgery being washed and hear the cry of the baby (Páez and Navarro 2012; Bakri et al. 2015) while general anesthesia was associated with discomfort, pain, nausea, and vomiting, among others (Tsen and Kodali 2010).
Limitation of the study
Only randomized clinical trials and observational study methods met the inclusion criteria for this study. Once more, the search elapsing was also limited to studies betwixt 2010 and 2019. Therefore, all these were limitations of the study.
Conclusion
In conclusion, both coldhearted techniques are reliable and well-tolerated for cesarean delivery. However, regional anesthesia emerged as a amend option for elective cesarean delivery. Regional anesthesia benefits for maternal and fetal outcome are superior to general anesthesia.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are bachelor on a formal request from the corresponding writer on reasonable request.
Abbreviations
- pH:
-
Potential of hydrogen
- GA:
-
General anesthesia
- RA:
-
Regional anesthesia
- SA:
-
Spinal anesthesia
- EA:
-
Epidural anesthesia
- CSE:
-
Combined spinal-epidural
- PDPH:
-
Post-dural puncture headache
- PRISMA:
-
Preferred Reporting Items for Systematic Review and Meta-Analysis
References
-
Abdallah MW, Elzayyat NS, Abdelhaq MM, Gado AAM (2014) A comparative study of general anesthesia versus combined spinal-epidural anesthesia on the fetus in cesarean section. Egyptian J Anaesth 30(ii):155–160
-
Açıkel A, Öztürk T, Göker A, Hayran GG, Keleş GT (2017) Comparison of patient satisfaction betwixt general and spinal amazement in emergency caesarean deliveries. Turk Anesteziyoloji ve Reanimasyon Dernegi Dergisi 45(1):41–46
-
Afolabi BB, Lesi FEA (2012) Regional versus general anaesthesia for caesarean section. Cochrane Database Syst Rev 10:89
-
Aksoy H, Aksoy Ü, Yücel B, Özyurt SS, Açmaz Grand, Babayiğit MA et al (2015) Blood loss in elective cesarean section: is there a difference related to the type of anesthesia? A randomized prospective study. J Turk German language Gynecol Assoc 16(iii):158
-
Aregawi A, Terefe T, Admasu W, Akalu 50 (2018) Comparing the effect of spinal and general anaesthesia for pre-eclamptic mothers who underwent caesarean delivery in a tertiary, Addis Ababa, Ethiopia. Ethiop J Health Sci 28(4):443–450
-
Arslantas R, Umuroglu T (2019) Comparing the furnishings of general and spinal anesthesia on the postoperative hurting intensity in patients undergoing emergent or elective cesarean section. Marmara Med J 32(two):62–67
-
Bakri MH, Ismail EA, Ghanem G, Shokry Grand (2015) Spinal versus general anesthesia for cesarean section in patients with sickle prison cell anemia. Korean J Anesthesiol 68(5):469
-
Blossom SL, Spong CY, Weiner SJ, Landon MB, Rouse DJ, Varner MW et al (2005) Complications of anesthesia for cesarean commitment. Obstet Gynecol 106(2):281–287
-
Caglar GS, Erdogdu P, Gursoy AY, Seker R, Demirtas S (2013) The touch on of route of anesthesia on maternal and fetal ischemia modified albumin levels at cesarean section: a prospective randomized written report. J Perinat Med 41(five):573–579
-
Chen Y, Liu West, Gong X, Cheng Q (2019) Comparison of effects of general anesthesia and combined spinal/epidural anesthesia for cesarean delivery on umbilical cord blood gas values: a double-bullheaded, randomized, controlled written report. Med Sci Monit 25:5272–5279
-
Devroe S, Van de Velde One thousand, King Southward (2015) Full general anesthesia for caesarean section. Curr Opin Anaesthesiol 28(3):240–246
-
Dyer RA, Els I, Farbas J, Torr GJ, Schoeman LK, James MF (2003) Prospective, randomized trial comparing full general with spinal anesthesia for cesarean commitment in preeclamptic patients with a nonreassuring fetal middle trace. Anesthesiology. 99(3):561–569
-
Edipoglu IS, Celik F, Marangoz EC, Orcan GH (2018) Issue of anaesthetic technique on neonatal morbidity in emergency caesarean section for foetal distress. PLoS One xiii(eleven):e0207388
-
Ghaffari Due south, Dehghanpisheh L, Tavakkoli F, Mahmoudi H (2018) The effect of spinal versus general anesthesia on quality of life in women undergoing cesarean delivery on maternal request. Cureus. 10(12):e3715
-
Harazim H, Stourac P, Blaha J, Grochova M, Klozova R, Noskova P et al (2019) The influence of mode of anaesthesia for caesarean commitment on neonatal Apgar scores in the Czech Commonwealth and Slovakia: secondary analysis of the results of an international survey in 2015. Biomedical Papers 163(ii):147–154
-
Havas F, Orhan Sungur M, Yenigun Y, Karadeniz M, Kilic Grand, Ozkan ST (2013) Spinal anesthesia for elective cesarean department is associated with shorter hospital stay compared to general anesthesia. Agri 25(2):55–63
-
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). Cochrane
-
Jain K, Bhardwaj N, Sharma A, Kaur J, Kumar P (2013) A randomised comparison of the effects of low-dose spinal or general anaesthesia on umbilical cord blood gases during caesarean delivery of growth-restricted foetuses with dumb Doppler period. Eur J Anaesthesiol 30(1):9–15
-
Kessous R, Weintraub AY, Wiznitzer A, Zlotnik A, Pariente G, Polachek H et al (2012) Spinal versus full general anesthesia in cesarean sections: the effects on postoperative hurting perception. Curvation Gynecol Obstet 286(1):75–79
-
Khan ZH, Eftekhar N, Barrak RS (2019) General versus spinal anesthesia during caesarean section; a narrative review. AACC. 5(1):18–21
-
Kim WH, Hur One thousand, Park SK, Yoo S, Lim T, Yoon HK et al (2019) Comparing between general, spinal, epidural, and combined spinal-epidural anesthesia for cesarean delivery: a network meta-analysis. Int J Obstet Anesth 37:5–fifteen
-
Kimber Craig SA (2019) Regional amazement for caesarean section and what to do if it fails. Anaesth Intens Care Med 8(8):320
-
Kolås T, Saugstad O, Daltveit A (2007) Planned cesarean versus planned vaginal commitment at term: comparing of newborn infant outcomes. Midirs Midwifery Digest 17(ii):267–268
-
Picayune SE, Orav EJ, Robinson JN, Caughey AB, Jha AK (2016) The relationship between variations in cesarean delivery and regional health care use in the United States. Am J Obstet Gynecol 214(half dozen):735.e1–735.e8
-
Madkour NM, Ibrahim SA, Ezz GF (2019) General versus spinal anesthesia during elective cesarean section in term low-hazard pregnancy as regards maternal and neonatal outcomes: a prospective, controlled clinical trial. Res Opin Anesth Intens Care vi(1):119
-
Mancuso A, De Vivo A, Giacobbe A, Priola V, Maggio Savasta L, Guzzo M et al (2010) General versus spinal amazement for elective caesarean sections: effects on neonatal short-term outcome. A prospective randomised study. J Matern Fetal Neonatal Med 23(10):1114–1118
-
Nguyen-Lu N, Carvalho JC, Kingdom J, Windrim R, Allen 50, Balki M (2016) Way of anesthesia and clinical outcomes of patients undergoing cesarean delivery for invasive placentation: a retrospective accomplice study of 50 consecutive cases. Can J Anaesth 63(xi):1233–1244
-
Páez LJJ, Navarro JR (2012) Regional versus general anesthesia for cesarean section commitment. Columb J Anesthesiology forty(iii):203–206
-
Sabol BA, Caughey AB (2016) Acidemia in neonates with a 5-minute Apgar score of seven or greater–what are the outcomes? Am J Obstet Gynecol 215(4):486.e1–486.e6
-
Saracoglu KT, Saracoglu A, Umuroglu T, Eti Z (2012) Neuraxial block versus general anaesthesia for cesarean department: post-operative pain scores and analgesic requirements. J Pak Med Assoc 62(5):441–444
-
Saygi AI, Ozdamar O, Gun I, Emirkadi H, Mungen E, Akpak YK (2015) Comparison of maternal and fetal outcomes among patients undergoing cesarean section under full general and spinal anesthesia: a randomized clinical trial. Sao Paulo Med J 133(three):227–234
-
Shek NW, Lao TT, Chan KK (2012) Mode of anaesthesia on fetal acrid-base condition at caesarean section. J Perinat Med forty(6):653–657
-
Shibli Grand, Russell I (2000) A survey of anaesthetic techniques used for caesarean section in the UK in 1997. Int J Obstet Anesth ix(3):160–167
-
Solangi SA, Khaskheli MS, Siddiqui MA (2012) Comparison of the effects of general vs spinal anesthesia on neonatal event. Anaesth Pain Intens Care:18–23
-
Staikou C, Tsaroucha A, Vakas P, Salakos N, Hasiakos D, Panoulis M et al (2013) Maternal and umbilical cord oxygen content and acid-base of operations residual in relation to full general, epidural or subarachnoid anesthesia for term constituent cesarean section. Clin Exp Obstet Gynecol 40(three):367–371
-
Sumikura H, Niwa H, Sato K, Nakamoto T, Asai T, Hagihira S (2016) Rethinking general anesthesia for cesarean section. J Anesth 30(two):268–273
-
Tsen LC, Kodali BS (2010) Can general anesthesia for cesarean commitment exist completely avoided? An anesthetic perspective. Expert Rev Obstet Gynecol 5(5):517–524
-
Yehuda Ginosar FR, Halpern Southward, Carl Weiner P (2013) Anesthesia and the fetus. Blackwell Publishing Ltd, United Kingdom, p 405
Acknowledgements
The authors would like to give thanks deeply all the members of the Section of Anesthesiology and Critical Care in both Imam Khomeini Infirmary Circuitous and Tehran University of Medical Sciences for their diverse back up during the flow of the report.
Writer information
Affiliations
Contributions
MI contributed to the report formulation and pattern, acquisition of the data, analysis, interpretation of the data, and drafting of the manuscript. ZHK contributed to the design of the written report, acquisition of the data, reporting of the result, and supervision of the whole process of the manuscript drafting and its critical revision. All authors read and approved the final manuscript.
Respective author
Ethics declarations
Ethics approval and consent to participate
Non applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional data
Publisher'south Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open up Access This article is licensed nether a Artistic Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long equally you lot give appropriate credit to the original author(s) and the source, provide a link to the Creative Eatables licence, and indicate if changes were fabricated. The images or other third party material in this article are included in the commodity's Creative Eatables licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Artistic Commons licence and your intended utilise is not permitted by statutory regulation or exceeds the permitted utilise, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/past/four.0/.
Reprints and Permissions
About this commodity
Cite this article
Iddrisu, M., Khan, Z.H. Anesthesia for cesarean delivery: general or regional anesthesia—a systematic review. Ain-Shams J Anesthesiol 13, one (2021). https://doi.org/10.1186/s42077-020-00121-vii
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s42077-020-00121-7
Keywords
- Regional anesthesia
- General anesthesia
- Cesarean delivery
- Spinal anesthesia
Source: https://asja.springeropen.com/articles/10.1186/s42077-020-00121-7
0 Response to "Cost of Delivering a Baby Cost of Annestesia"
Post a Comment